Practicing physicians are always vulnerable to malpractice litigation. The threat of litigation, unfortunately, leads to defensive practice, which in turn adds billions to the cost of healthcare. Defensive practice is also unsafe for patients. This fear of litigation affects the daily practice of physicians and also the quality of life outside the clinic.
What constitutes Malpractice?
In order to be held liable for a malpractice suit, there are four elements that need to be proved:
- The physician had a duty.
- The physician breached that duty.
- The patient was harmed.
- The harm was caused due to the physician’s breach of duty.
The physician cannot be held liable if all the four conditions are not met. However, there are certain cases where even if the four conditions are met, the physician cannot be held liable for malpractice.
Assumption of Risk
Mrs. Schneider was diagnosed with a breast lump, and was asked to get it surgically removed. However, she decided to undergo treatment under Dr. Revici, using non-traditional, non-invasive and non-toxic methods. She subsequently developed breast cancer that spread and required bilateral mastectomy. Mrs. Schneider sued Dr. Revici for medical malpractice, but the consent forms that were signed by her, stated that she was aware of the risks involved in refusing conventional treatment and agreeing to Dr. Revici’s method of treatment. The court ruled in favor of Dr. Revici, stating the expressed assumption of risk as a valid defense.
Assumption of risk lies in the adage ‘volenti non fit injuria’– to a willing person, no injury is done. Under this, the plaintiff’s implied or expressed agreement absolves the defendant from responsibility. It is very important to communicate the risks involved to the patient and obtain their consent to the line of treatment. Physicians can reduce the chance of litigation if the patient is aware of the risks, benefits and alternatives before the procedure and then decide to “assume the risk”.
Good Samaritan
Ms. McCain impaled her leg on a rebar at a construction site. Dr. Baston responded to her call for help and after cleaning the wound, asked her to seek medical care immediately. However, Ms. McCain waited for a week before going to a clinic and by then she required surgical management for the infected wound. Dr. Baston was sued by Ms. McCain for poor treatment. The court did not find Dr. Baston liable for damages, as he had acted as a Good Samaritan.
The Good Samaritan law is made to protect physicians who respond to an emergency situation. Under this law, a physician responding to an emergency is protected from being held liable for injuries or damages that occur during the emergency. There are, however, certain caveats in the use of the Good Samaritan law. It requires the following conditions to be met:
- The incident is an emergency.
- The act of rendering care is voluntary.
- The patient accepts the care received.
- The care is provided in good faith, intended to help.
- The care provider receives no remuneration for the care provided.
- The care provided cannot be grossly negligent.
The Good Samaritan defense was extended to in-hospital settings also, after the McKenna v. Cedars of Lebanon Hospital case. However, the Good Samaritan defense for in-hospital settings varies from state to state.
Contributory Negligence
Despite being informed by Dr. Hull to delay scalp reduction, Mr. Smith, who underwent hair implants over several years, signed the consent forms and underwent surgery. Unhappy with the scarring on his head, Mr. Smith sued Dr. Hull for malpractice. The court ruled in favor of Dr. Hull as according to them, Mr. Smith knowingly underwent the surgery at his own peril, which amounted to contributory negligence.
According to the concept of contributory negligence, a person is responsible for their own action or inaction, which, if contributes to the negligence, then the person should not be awarded damages. Contributory negligence may be used as a defense when a patient demands procedures or treatments against the physician’s advice.
Comparative fault
Dr. Azzara found Mrs. Ostrowski’s toenail producing draining, red in color and painful to touch. In the course of her treatment, Dr. Azzara removed he toe nail to facilitate drainage. However, Mrs. Ostrowski, who was a hypertensive diabetic, had poor weight, diet and health management habit, did not heal and her toe became a non-healing pre-gangrenous wound. She sued Dr. Azzara and a vascular surgeon testified that removal of the toe nail was unnecessary. Dr. Azzara, in his defense, was able to prove that Mrs. Ostrowski’s smoking and poor health management contributed to the outcome. The court found her to be 51% at fault and Dr. Azzara at 49%. The jury ruled in favor of Dr. Azzara and no damages were awarded.
Comparative fault is similar to comparative negligence, except, that in the case of comparative fault; a patient might be awarded some damages, depending on the percentage of contribution by the patient and the physician to the outcome of the treatment.
What physicians need to know?
Clinical defenses as stated above have been and can be used in malpractice cases, even if the four elements of duty are present. Physicians need to know about these defenses to optimize and reduce the risk of liability if confronted with a potential malpractice suit, rather than practice defensive medical procedures or treatments.
References
- Bowen Berry, J. (2001, January 14). The physician’s guide to medical malpractice. Retrieved January 21, 2016, from http://www.ncbi.nlm.nih.gov: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1291321/
- Defenses to Medical Malpractice. (2016). Retrieved January 21, 2016, from http://www.injury.findlaw.com: http://injury.findlaw.com/medical-malpractice/defenses-to-medical-malpractice-patients-negligence.html
- Michael Jason Hudson, M., & Gregory P. Moore, M. J. (2011). Defenses to Malpractice. Retrieved January 21, 2016, from http://www.medscape.com: http://www.medscape.com/viewarticle/755818
- Sandy Sanbar, M. P. (2006). Medical Malpractice Defenses. In MedMal Survival Handbook (pp. 257-267).
- Suszek, A. (2016). Types of Defenses in a Medical Malpractice Case. Retrieved January 21, 2016, from http://www.alllaw.com: http://www.alllaw.com/articles/nolo/medical-malpractice/defense-2.html




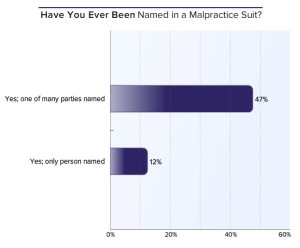 The survey showed that 59% of respondents have been named in at least one malpractice suit. While nearly half (47%) were named in the suit along with others, 12% were the only parties sued.
The survey showed that 59% of respondents have been named in at least one malpractice suit. While nearly half (47%) were named in the suit along with others, 12% were the only parties sued.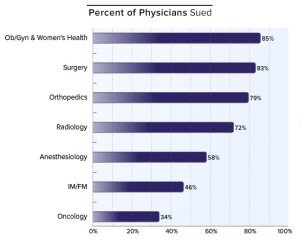 85% of obstetricians/ gynecologists, 83% of general surgeons, and 79% of orthopedists have been sued.
85% of obstetricians/ gynecologists, 83% of general surgeons, and 79% of orthopedists have been sued. 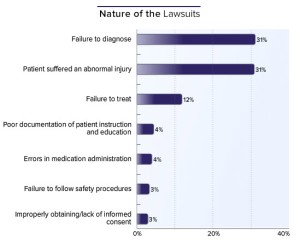 Respondents were asked to check as many options as were relevant, to the question about the nature of their lawsuits. The highest numbers of suits (31%) were related to a failure to diagnose and patient suffering abnormal injuries. Failure to treat (12%) came in at third place and was far behind the first two. Less than 5% of respondents cited poor documentation or medication errors (both 4%) or failure to follow safety procedures or obtain informed consent (both 3%).
Respondents were asked to check as many options as were relevant, to the question about the nature of their lawsuits. The highest numbers of suits (31%) were related to a failure to diagnose and patient suffering abnormal injuries. Failure to treat (12%) came in at third place and was far behind the first two. Less than 5% of respondents cited poor documentation or medication errors (both 4%) or failure to follow safety procedures or obtain informed consent (both 3%).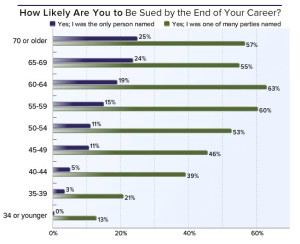 least one malpractice suit by the time they were 54 years old. With physicians at 60 years of age, this percentage rose to about 80%. However, those who responded to this question, tended to be in specialties that had a higher likelihood of being sued. As one respondent in the Medscape survey wrote, “The older you get, the more you have to lose.”
least one malpractice suit by the time they were 54 years old. With physicians at 60 years of age, this percentage rose to about 80%. However, those who responded to this question, tended to be in specialties that had a higher likelihood of being sued. As one respondent in the Medscape survey wrote, “The older you get, the more you have to lose.”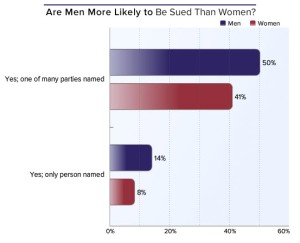 While nearly two thirds (64%) of male respondents were sued as compared to less than half of women (49%); men were also sued more as the only named defendant in a suit (14%) as compared to women (8%).
While nearly two thirds (64%) of male respondents were sued as compared to less than half of women (49%); men were also sued more as the only named defendant in a suit (14%) as compared to women (8%).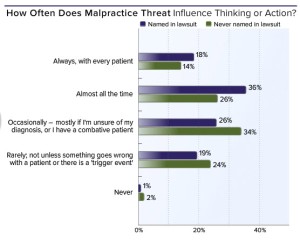 threat of another lawsuit affects them either always, with every patient (18%) or almost all the time (36%). 19% percent were rarely bothered, unless something went wrong with the patient or there was a trigger event.
threat of another lawsuit affects them either always, with every patient (18%) or almost all the time (36%). 19% percent were rarely bothered, unless something went wrong with the patient or there was a trigger event.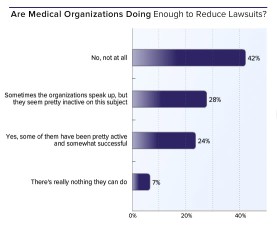
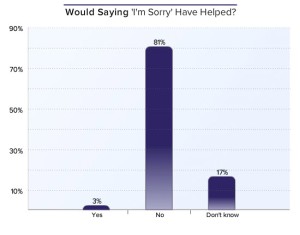
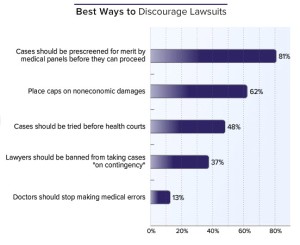 Roughly about half (48%) believed that cases should be tried before a health court. Among verbal suggestions, unsurprisingly, many urged tort reform. However, by far the most popular suggestion, particularly among male respondents, was to make the losing side pay. A larger number of women respondents as compared to the men mentioned improved communication with patients as a way to discourage lawsuits.
Roughly about half (48%) believed that cases should be tried before a health court. Among verbal suggestions, unsurprisingly, many urged tort reform. However, by far the most popular suggestion, particularly among male respondents, was to make the losing side pay. A larger number of women respondents as compared to the men mentioned improved communication with patients as a way to discourage lawsuits.
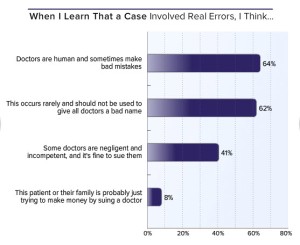 Most physicians showed sympathy for colleagues who are sued, even in cases that involve actual errors.
Most physicians showed sympathy for colleagues who are sued, even in cases that involve actual errors.
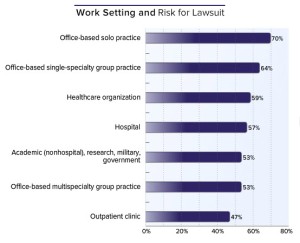 Malpractice suits in office-based solo practices (70%) or single-specialty groups (64%) were found to be the highest. The second lowest percentage (53%) reported were in office-based multispecialty groups. Surprisingly, the least likely to face lawsuits (47%) were outpatient clinics.
Malpractice suits in office-based solo practices (70%) or single-specialty groups (64%) were found to be the highest. The second lowest percentage (53%) reported were in office-based multispecialty groups. Surprisingly, the least likely to face lawsuits (47%) were outpatient clinics.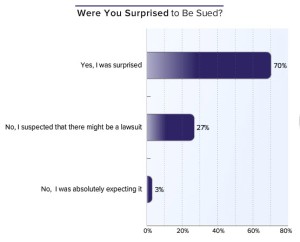
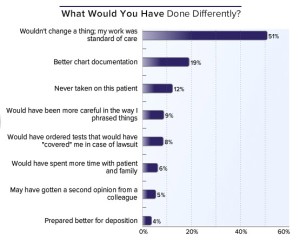
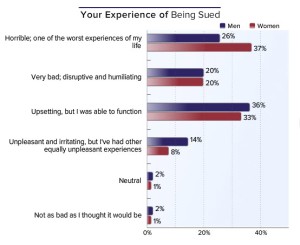 When asked to verbalize their experiences, physicians typically described feelings of betrayal by patients, humiliation, and disillusionment with the legal system. As one physician said, “The evils of human nature on display: greed, dishonesty, corruption. Clever arguments in the court trumps truth.”
When asked to verbalize their experiences, physicians typically described feelings of betrayal by patients, humiliation, and disillusionment with the legal system. As one physician said, “The evils of human nature on display: greed, dishonesty, corruption. Clever arguments in the court trumps truth.”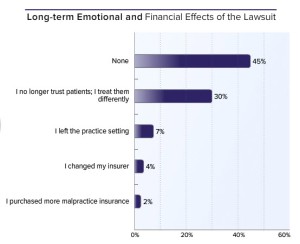 While less than half of respondents reported no long-term emotional or financial effects,the malpractice suit had a negative effect on trust for 30% of physicians.Some expressed their desire to improve professional behaviour, more documentation and connecting better with patients. A large number of physicians mentioned long-term anxiety, depression, and suffering in general as fallout of being sued.
While less than half of respondents reported no long-term emotional or financial effects,the malpractice suit had a negative effect on trust for 30% of physicians.Some expressed their desire to improve professional behaviour, more documentation and connecting better with patients. A large number of physicians mentioned long-term anxiety, depression, and suffering in general as fallout of being sued. Of all of the long-term effects expressed in this survey, perhaps the most disturbing was the negative impact lawsuits have on the physician-patient relationship. Most physicians said that they had stopped trusting patient’s responses to their quality of work.
Of all of the long-term effects expressed in this survey, perhaps the most disturbing was the negative impact lawsuits have on the physician-patient relationship. Most physicians said that they had stopped trusting patient’s responses to their quality of work.





